Midfoot Arthritis Diagnosis and Treatment
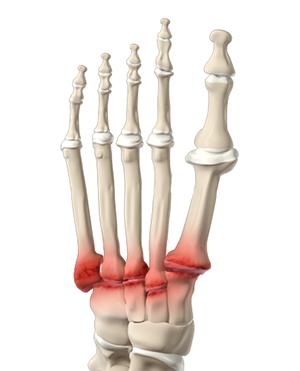
What is Midfoot Arthritis?
Midfoot arthritis is pain and inflammation of the midfoot. It occurs due to damage of cartilage or tissues around the joints. The damage may occur due to injury, aging or autoimmunity. The midfoot consists of 5 bones called lesser tarsal bones. They are:
- Cuboid
- Navicular
- Medial Cuneiform
- Intermediate Cuneiform
- Lateral Cuneiform
Symptoms of Midfoot Arthritis
The symptoms of midfoot arthritis include:
- A bony prominence on your midfoot
- Pain and inflammation that aggravates on standing or walking
- Gradual or sudden pain with a feeling of discomfort
- Tenderness around the affected joints
- Pain with first few steps after getting up in the morning
Diagnosis of Midfoot Arthritis
Your doctor physically examines your midfoot for pain and inflammation. The exact location and severity of the pain are essential to identify the type and the extent of the damage. Your doctor will also take your medical history and may order an X-ray or CT-scan or MRI to confirm the diagnosis.
Treatment of Midfoot Arthritis
Non-Surgical Methods
The non-surgical treatment options include:
- Pain medicines and anti-inflammatory drugs injections
- Wearing comfortable shoes with rocker bottom
- Avoiding excess strain to the affected foot
- Cross training such as swimming and stationary bike with appropriate stiff soled bike shoe
Selective Injections
- Small dose of steroid reduces inflammation
- Hyaluronic Acid (HA) or carbo-protein that preserves cartilage.
- Platelet Rich Plasma (PRP): preserves cartilage and decreases inflammation
Surgical Treatments
The bones that are causing the foot pain are arthrodeised surgically by a midfoot fusion to eliminate the rubbing of bones against each other. Midfoot fusion involves the following steps:
- The length of the incision made by your surgeon depends on the number of bones that need to be fused.
- The damaged cartilage and soft tissue are removed.
- Care is taken to prevent damage to healthy tendons, ligaments or nerves of the foot during the surgery.
- Graft tissue is often used, along with your own stem cells to fill the damaged tissue. The graft may be autograft (taken from your body), allograft (from a donor) or synthetic material.
- The bones are fused with screws, staples, metal implants or plates.
- The incision is closed, and the foot is covered with a bandage.
Recovery after Surgery
- Your foot will be placed in a cast for about 6 to 10 weeks. You may need to use a walker.
- You will be encouraged to keep weight off your leg.
- You are not allowed to perform any activity that may stress your foot for about 2 to 3 weeks.
- Physiotherapy exercises will be taught to enhance your flexibility, range of motion and strength.
Complications of Surgery
Complications are rare. Possible complications of midfoot fusion surgery include:
- Bones do not fuse (smoking is a possible cause)
- Healing takes longer than usual
- Infection
- Formation of blood clots
- Damage to nerves